
Resolution of a rare case of hypercalcemia in a PTHrp-producing pancreatic neuroendocrine tumor using selective internal radiation therapy with 90Y microspheres
Highlight box
Key findings
• Patient with pancreatic neuroendocrine tumor (PNET) experiences stabilization of calcium levels through treatment of liver metastasis with 90Y labelled microspheres.
What is known and what is new?
• There are several lines of treatment for hypercalcemia caused by parathyroid hormone-related peptide (PTHrp) producers PNETs, where surgery is the Gold standard.
• The possibility of treatment of hypercalcemia refractory to the usual treatments and surgery of the tumor is being studied.
What is the implication, and what should change now?
• PTHrp produced by PNET is a very rare case of disease, demanding the right tools to correct hypercalcemia. Therefore, it is a treatment that could be considered for other cases.
Introduction
Background
Many authors explain that the management of the hypercalcemia associated with paraneoplastic syndrome can be difficult and, in the case of pancreatic neuroendocrine tumor (PNET), may require direct antitumor therapy and the surgical intervention with removal of the source of parathyroid hormone-related peptide (PTHrp) secretion should be considered the gold standard for permanent correction of hypercalcemia in patients with operable tumor (1,2).
Other authors recommend somatostatine analogues and hepatic artery embolisation as options for metastases (2).
In unresecable or incompletely resected cases, conventional chemotherapy, typically regimens including capecitabine or temozolomide have been applied for symptomatic control (1).
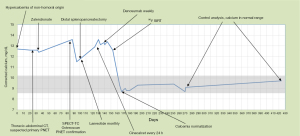
In our case, neither surgery of the primary tumor of the pancreas, nor the lines of drug treatment (zalendronate, lanreotide, cinacalcet and denosumab) resolved the hypercalcemia, because de liver metastases (the larger of 8 cm) was the PTHrp-producer, so calcium levels normalized after selective internal radiation therapy (SIRT).
SIRT is a therapeutic procedure that uses biocompatible resin microspheres labelled with 90Y (pure beta emitter). It is indicated for hepatocarcinoma not amenable to surgical resection, liver transplantation and ablative therapies. It is also suitable for patients on the waiting list for liver transplant, for recurrence of hepatocarcinoma in transplant patients and unresectable liver metastases, especially of colorectal origin (3,4).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
The patient, a woman in her 60s, visited her primary care physician due to persistent asthenia of 6 months of evolution, accompanied by prolonged somnolence of up to 11–12 hours a day, weight loss of up to 6 kg and severe constipation (up to 12 days without bowel movement). With these symptoms, she was referred to Endocrinology and moderate hypercalcemia of 12.7 mg/dL (normal 8.6–10.2 mg/dL) was detected in the blood test. The initial physical examination showed no significant abnormalities.
In successive laboratory tests to evaluate the cause of hypercalcemia, low PTH levels of 10 pg/mL (normal 15–65 pg/mL) and 25-hydroxyvitamin D 9 ng/mL (insufficiency ˂30 ng/mL), and very high values of PTHrp 62.6 pmol/L (normal ˂1.5 pmol/L) observed.
In the presence of hypercalcemia with suppressed PTH, a provisional diagnosis of moderate non-hormonal hypercalcemia was considered. Two lesions in the liver parenchyma were observed by thoraco-abdominal computed tomography (CT), together with a 10 cm × 8 cm tumor in the pancreatic body. This tumor showed intense vascularization and marked contrast uptake, which led to a suspicion of a functioning PNET, presumably a PTH-rp producer with hepatic metastases. In order to obtain a more accurate histological evaluation, a liver biopsy was performed, which confirmed the positivity of neoplastic cells for specific markers, such as synaptophysin and chromogranin. The cell proliferation index was moderate, with an approximate Ki67 of 10%. PTHrp levels remained elevated, recording PTHrp 62.6 pmol/L (normal ˂1.5 pmol/L). Subsequently, the patient was referred to the Nuclear Medicine Department for a more exhaustive study. A full body bone scan was performed by administering the radiopharmaceutical 99mTc-HDP, which showed no alterations suggestive of bone metastases.
A Single-photon emission computed tomography-CT (SPECT-CT) was then performed with 111In-Octreotide, which showed a high uptake of the radiopharmaceutical (Krenning score 4) in the voluminous tumor of the pancreatic body and in the liver lesions, indicating a high overexpression of SSTR. The final diagnostic information was a 10 cm neuroendocrine tumor of pancreatic origin, classified as grade 2 (G2), with a Ki proliferation rate of 10%, 8 cm PTHrp-producing liver metastases, and high somatostatin receptor overexpression at both pancreatic and hepatic levels (Figure 1).

By means of liver biopsy and imaging studies, the above-mentioned definitive diagnosis was established as opposed to the provisional diagnosis of severe non-hormonal hypercalcemia.
To mitigate hypercalcemia while awaiting definitive diagnosis, on day 91 after the first consultation, treatment with zalendronate was started, obtaining a decrease in calcium levels, but not normalization, going from 13.6 mg/dL previously to 11.5 mg/dL. On day 95, lanreotide was added to the treatment.
After an exhaustive evaluation by a multidisciplinary committee specialized in digestive tumors, a combined therapeutic plan was determined, based on the removal of the primary tumor through splenopancreatectomy, and the continued treatment of hepatic metastases with 90Y for subsequent surgical removal.
On the 101st day, the patient underwent a distal splenopancreatectomy as a key part of her treatment. During this procedure, tissue samples were taken and subsequently sent to the pathology laboratory. The results confirmed the presence of a well-differentiated neuroendocrine tumor in the pancreas, with an extension to the liver (TNM stage: pT3 pN0 pM1a). No evidence of tumor infiltration of the spleen or gallbladder was identified.
After planning with 99mTc-labelled albumin macroaggregates in order to evaluate the hepatic circulation and a possible hepato-pulmonary shunt (Figure 2), SIRT was performed on day 153 with a dose of 5 GBq of 90Y-microspheres.

The next day after treatment with SIRT, resolution of tumoral hypercalcemia was biochemically confirmed with negative PTHrp (˂1.5 pmol/L). These calcium levels remained in the normal range (9.3 mg/dL) until day 270 when the last consultation was performed (9.1 mg/dL).
The patient attended her usual follow-up 6 months after her last blood test and calcium levels are still in the normal range of 9.7 mg/dL (Figure 3).
Following splenopancreatectomy and SIRT, radiological evaluation showed a marked improvement in the patient’s condition. The segmentally treated liver metastases underwent significant changes were found, observing a rounded hypercaptating area with cystic/necrotic-appearing zones, which could indicate a post-treatment vascular lesion. A small hypervascular lesion was detected in segment V, quite stable compared to the previous CT scan, although its exact nature could not be determined.
Discussion
PNETs are very rare neoplasms originating in neural crest cells, with an incidence of 1.8 and 2.6 per 100,000 persons for women and men respectively (5). Therefore, hypercalcemia due to PTHrp in the context of a pancreatic neuroendocrine tumor is even rarer, estimated by Kamp et al. at 1.1% in a series of 895 patients (6).
On the other hand, PTHrp plays a central role in malignant tumor hypercalcemia, which is one of the most common paraneoplastic syndromes. PTHrp produced by the tumor acts through a common PTH/PTHrp receptor to promote bone resorption, inhibit calcium excretion by the kidney and induce hypercalcemia (7).
In our case, treatment is initiated with the administration of bisphosphonates (zalendronate), which constitute the first-line treatment for hypercalcemia (8). Faced with an inadequate pharmacological response, the second-line treatment for addressing calcium levels is chosen through the use of somatostatin analogs (lanreotide, 60 mg monthly). Confidence in this treatment is supported by the verification of overexpression of somatostatin receptors SSTR2 and SSTR5 in the PNET (7-10).
On the same day, he underwent a splenopancreatectomy. Following worsening hypercalcemia, a decision is made to initiate treatment with Cinacalcet. This is a calcimimetic that directly decreases PTH levels by increasing the sensitivity of the calcium-sensing receptor to extracellular calcium, which leads to a decrease in serum calcium levels (11-13).
Denosumab was added to the treatment without achieving normalization of blood calcium levels. Denosumab is a monoclonal antibody with affinity for RANKL. Blocking RANKL prevents the maturation, function and survival of osteoclasts and thus decreases bone resorption (14).
Six months after the date of diagnosis, the patient was admitted for treatment of the larger liver metastasis 8 cm in diameter by administration of 90Y labelled microspheres, receiving a dose of 5 GBq (with a tumor dose of 447.56 Gy and 28.94 Gy in healthy liver tissue).
SIRT is based on the dual hepatic vascularization, liver tumors have a predominantly arterial flow, while the flow of healthy liver parenchyma is mostly portal (80%). Thus, by depositing the microspheres in the arterial circulation, the radiation received by the healthy tissue is minimal relative to the tumor tissue, making it possible to deliver high doses of radiation to the tumor safely. The microspheres become trapped in the capillary bed of the tumor and the beta radiation from 90Y destroys the tumor cells close to these capillaries. This is a mechanism of free radical generation by ionization of water molecules causing permanent DNA damage and apoptosis of the tumor cells (15).
The half-life of 90Y is approximately 64.2 hours and almost 90% of the beta particles are emitted within 7 days. This beta radiation can penetrate liver tissue to an average depth of 2.5 mm with minimal irradiation of healthy tissue and nearby organs (16).
Another line of treatment described in the literature is radionuclide therapy, e.g., 177Lu-octreotate with affinity for SSRT. It is used in some inoperable cases with normalization of calcium levels, improvement of symptoms and survival (6,17-19).
There are other targeted therapies such as sunitinib, a potent tyrosine kinase inhibitor, which has shown some efficacy in calcium reduction in clinical cases (6,20,21).
Finally, everolimus, an inhibitor of the target rapamycin has shown some utility in the control of non-PNET tumors, in non-PNET carcinoid syndromes. However, it has not been studied in the control of hypercalcemia yet (22).
As hypercalcemia is a potentially life-threatening condition and patients might not have any symptoms or non-specific symptoms, we should keep a high suspicion for the diagnosis. Rapid initiation of general treatment is essential for a good prognosis. Early diagnosis is key both for the management of hypercalcemia and for diagnosing and treating the cause of hypercalcemia, as in the case presented in our study, where detecting hypercalcemia has led to the diagnosis of PNET and its liver metastases.
Conclusions
In conclusion, SIRT with 90Y microspheres could be another therapeutic option to be taken into account in the case of hepatic metastases producing PTHrp that cause hypercalcemia resistant to other lines of treatments. However, more research is needed on the application of SIRT with 90Y microspheres in the management of hypercalcemia secondary to PNET-producing PTHrp.
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at https://apc.amegroups.com/article/view/10.21037/apc-23-19/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apc.amegroups.com/article/view/10.21037/apc-23-19/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ferrel B, Franko J, Tee MC. Rare case of pancreatic neuroendocrine tumour presenting as paraneoplastic hypercalcaemia. BMJ Case Rep 2021;14:e240786. [Crossref] [PubMed]
- Papazachariou IM, Virlos IT, Williamson RC. Parathyroid hormone-related peptide in pancreatic neuroendocrine tumours associated with hypercalcaemia. HPB (Oxford) 2001;3:221-5. [Crossref] [PubMed]
- Kim HC. Radioembolization for the treatment of hepatocellular carcinoma. Clin Mol Hepatol 2017;23:109-14. [Crossref] [PubMed]
- Salem R, Lewandowski RJ, Kulik L, et al. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology 2011;140:497-507.e2. [Crossref] [PubMed]
- Halfdanarson TR, Rabe KG, Rubin J, et al. Pancreatic neuroendocrine tumors (PNETs): incidence, prognosis and recent trend toward improved survival. Ann Oncol 2008;19:1727-33. [Crossref] [PubMed]
- Kamp K, Feelders RA, van Adrichem RC, et al. Parathyroid hormone-related peptide (PTHrP) secretion by gastroenteropancreatic neuroendocrine tumors (GEP-NETs): clinical features, diagnosis, management, and follow-up. J Clin Endocrinol Metab 2014;99:3060-9. [Crossref] [PubMed]
- Sato K, Onuma E, Yocum RC, et al. Treatment of malignancy-associated hypercalcemia and cachexia with humanized anti-parathyroid hormone-related protein antibody. Semin Oncol 2003;30:167-73. [Crossref] [PubMed]
- Saunders Y, Ross JR, Broadley KE, et al. Steering Group. Systematic review of bisphosphonates for hypercalcaemia of malignancy. Palliat Med 2004;18:418-31. [Crossref] [PubMed]
- Castinetti F, Saveanu A, Morange I, et al. Lanreotide for the treatment of acromegaly. Adv Ther 2009;26:600-12. [Crossref] [PubMed]
- Oberg K, Kvols L, Caplin M, et al. Consensus report on the use of somatostatin analogs for the management of neuroendocrine tumors of the gastroenteropancreatic system. Ann Oncol 2004;15:966-973. [Crossref] [PubMed]
- Goldner W. Cancer-Related Hypercalcemia. J Oncol Pract 2016;12:426-32. [Crossref] [PubMed]
- Muller I, Premawardhana LD. Hypercalcaemia with undetectable parathormone levels. BMJ 2018;363:k4074. [Crossref] [PubMed]
- O'Callaghan S, Yau H. Treatment of malignancy-associated hypercalcemia with cinacalcet: a paradigm shift. Endocr Connect 2021;10:R13-24. [Crossref] [PubMed]
- Thosani S, Hu MI. Denosumab: a new agent in the management of hypercalcemia of malignancy. Future Oncol 2015;11:2865-71. [Crossref] [PubMed]
- Choi JW, Kim HC. Radioembolization for hepatocellular carcinoma: what clinicians need to know. J Liver Cancer 2022;22:4-13. [Crossref] [PubMed]
- Salem R, Lewandowski RJ, Sato KT, et al. Technical aspects of radioembolization with 90Y microspheres. Tech Vasc Interv Radiol 2007;10:12-29. [Crossref] [PubMed]
- Kanakis G, Kaltsas G, Granberg D, et al. Unusual complication of a pancreatic neuroendocrine tumor presenting with malignant hypercalcemia. J Clin Endocrinol Metab 2012;97:E627-31. [Crossref] [PubMed]
- Iliuta IA, Beauregard JM, Couture F, et al. Reversal of Severe and Refractory Humoral Hypercalcemia With 177Lu-Octreotate Peptide Receptor Radionuclide Therapy for Neuroendocrine Tumor of the Pancreas. Clin Nucl Med 2015;40:e448-50. [Crossref] [PubMed]
- Bergsma H, van Vliet EI, Teunissen JJ, et al. Peptide receptor radionuclide therapy (PRRT) for GEP-NETs. Best Pract Res Clin Gastroenterol 2012;26:867-81. [Crossref] [PubMed]
- Karaca H, Lale A, Dikilitas M, et al. Recovery of paraneoplastic hypercalcemia by sunitinib treatment for renal cell carcinoma: a case report and review of the literature. Med Oncol 2010;27:1023-6. [Crossref] [PubMed]
- Valdes-Socin H, Almanza MR, Fernández-Ladreda MT, et al. Use of cinacalcet and sunitinib to treat hypercalcaemia due to a pancreatic neuroendocrine tumor. Arch Endocrinol Metab 2017;61:506-9. [Crossref] [PubMed]
- Bainbridge HE, Larbi E, Middleton G. Symptomatic Control of Neuroendocrine Tumours with Everolimus. Horm Cancer 2015;6:254-9. [Crossref] [PubMed]
Cite this article as: Dobra Neacsu E, Martínez Montalbán E, Martínez de Miguel B. Resolution of a rare case of hypercalcemia in a PTHrp-producing pancreatic neuroendocrine tumor using selective internal radiation therapy with 90Y microspheres. Ann Pancreat Cancer 2024;7:5.


